Major step towards individual cancer immunotherapy
Medicine has great hopes for personalised cancer immunotherapy. The idea is to have a vaccine prompt the immune system to fight a tumour. Scientists at ETH Zurich have developed a method that allows them to determine which molecules are suited to patient-specific immunisation.
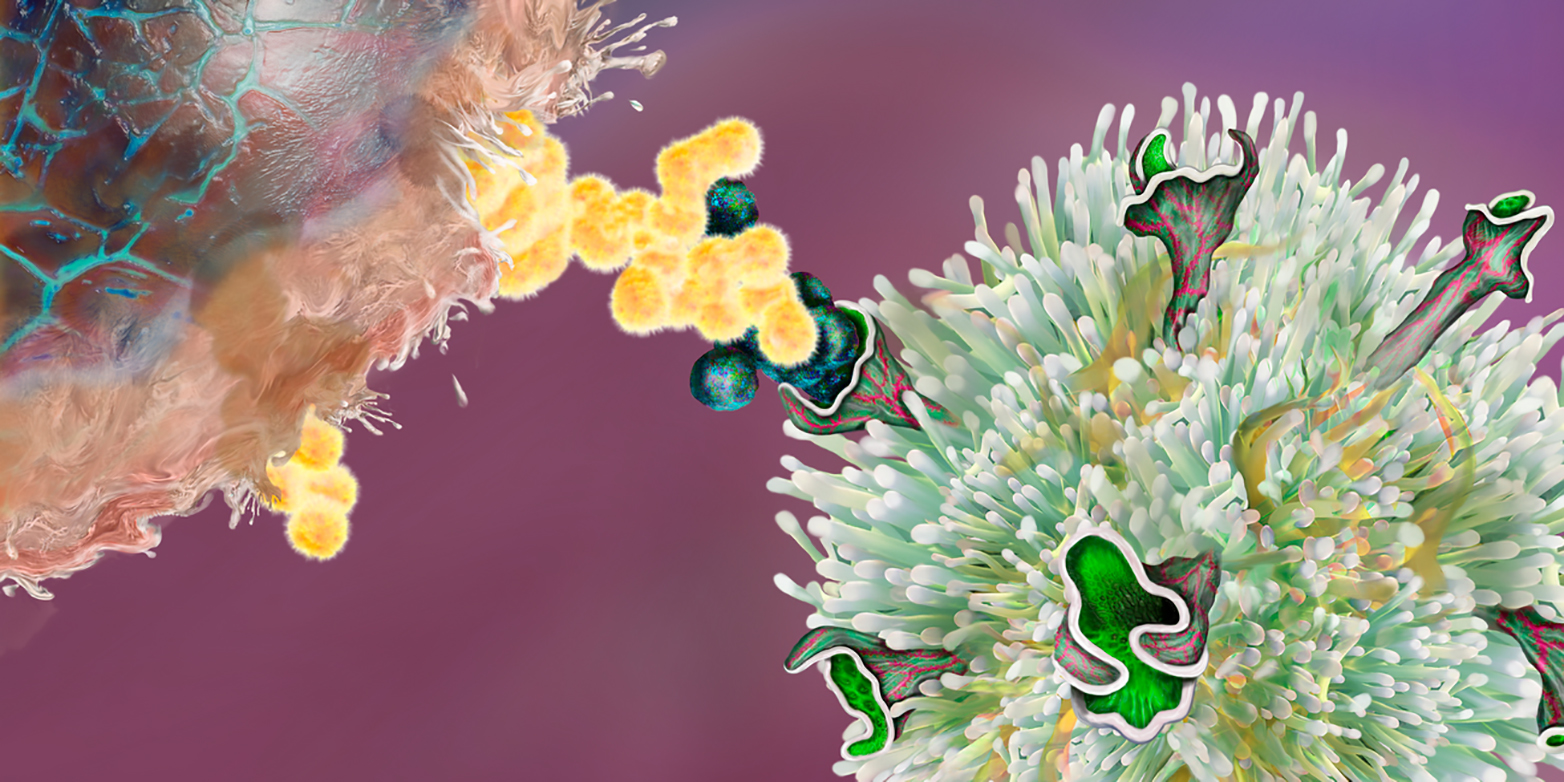
Cells belonging to the body’s own immune system can help fight tumours. For several years now, this has allowed oncologists to use medications known as checkpoint inhibitors to encourage T cells to eliminate tumour cells. Last year the two scientists who discovered this therapeutic approach were awarded the Nobel Prize for Medicine.
While doctors are enjoying some initial successes with this method, especially with regard to melanomas and several other types of cancer, immunologists and cancer researchers are working to develop the approach further. What they have in mind is a vaccine that would cause cancer-repelling T cells to multiply in the body, thereby strengthening the body’s immune defences. The big question is which molecules are suitable for a vaccine? Researchers working in the team of Manfred Kopf, Professor of Molecular Biomedicine, have now developed a method for identifying such molecules.
Since on the one hand tumours differ greatly from patient to patient, and on the other no two people (except identical twins) have the same immune system, future immunisation against cancer is a complex example of personalised medicine. The goal is to develop an individual vaccine for each patient.
Potential vaccines include pieces of proteins, known as peptides, that are found only in tumours due to a mutation. Because T cells are specific and always recognise only one particular peptide, just as a key fits only one lock, a further prerequisite for a vaccine of this kind is that the patient has T cells capable of recognising these cancer peptides in the first place. So before doctors can immunise a cancer patient, laboratory tests must be conducted to search for corresponding pairs of T cells and peptides. A peptide that is recognised by a T cell can be used for personalised immunisation. The vaccine should then activate the T cells in the body that recognise only that peptide (and thus tumour cells). These T cells should ultimately wipe out the tumour.
The ETH researchers’ method makes it possible for a laboratory to determine which T cells recognise which peptide. Up to now this has been incredibly difficult. The scientists used tumours in mice to show that their approach works. Next, they want to demonstrate the effectiveness of their approach in dealing with tumours in humans.